Transverse Myelitis
Acute Transverse Myelopathy and back pain
Learn about this neurological condition and how it is managed.
What is transverse myelitis?
Acute transverse myelopathy (ATM) is a clinical definition of an acute neurologic condition that reflects impairment of spinal cord function. The spinal cord is the part of your central nervous system that runs through the spine from the brain. Nerves branch off of your spinal cord to innervate organs, muscles, skin, connective tissues and fascia. These nerves are responsible for motor function, sensory function, reflexes, organ function and etc.
Transverse Myelitis (TM) is a disorder caused by inflammation of the spinal cord. It is characterized by symptoms and signs of neurologic dysfunction in motor and sensory tracts on both sides of the spinal cord. The involvement of motor and sensory control pathways frequently produce altered sensation, weakness and sometimes urinary or bowel dysfunction.
The term "myelopathy" has a different meaning from "myelitis", even if the words are often confused. Both terms indicate spinal cord involvement by some pathological event; while myelopathy does not imply any etiological factor, myelitis refers to inflammatory diseases of the spinal cord. Magnetic resonance imaging is the modality of choice for diagnosis.
What are the symptoms of transverse myelitis?
There are four classic symptoms of transverse myelitis:
weakness in the arms/legs may progress over hours to up to four weeks, this can progress to paraparesis or paraplegia
sensory symptoms such as numbness or tingling
pain and discomfort
bladder dysfunction and/or bowel motility problems including constipation, incontinence, and urgency
The cause of 60% of transverse myelitis cases may remain unknown despite the presence of inflammatory mechanisms. In this regard it would be considered idiopathic. However, the remaining 40% is associated with autoimmune disorders such as multiple sclerosis, neuromyelitis optica, systemic lupus erythematous, Sjogren’s syndrome and sarcoidosis among others.
There is no age group or specific demographic that is more prone developing transverse myelitis, it strikes all age groups — from young children to the elderly — regardless of family history, gender or race. In younger patients, transverse myelitis may be the first indication of disorders such as multiple sclerosis or neuromyelitis optica.
Can you recover from transverse myelitis?
Recovery from transverse myelitis is often at least partial with the biggest results occurring within the firs three months following an acute episode. Some patients may make near full to full recovery gains with little to no long term problems. Some may have permanent disabilities that will affect their ability to live normal lives. Depending on whether or not a patient has underlying autoimmune or rheumatological issues, transverse myelitis could be a one time occurrence or be a re-occurring problem.
Treatments for transverse myelitis
Transverse myelitis is a condition that has no cure. However the condition can be treated to manage symptoms, halt progression, and reduce permanent disability and symptoms. Medical treatments are designed to target underlying conditions, reduce spinal cord inflammation, address infections that cause the condition, and control symptoms.
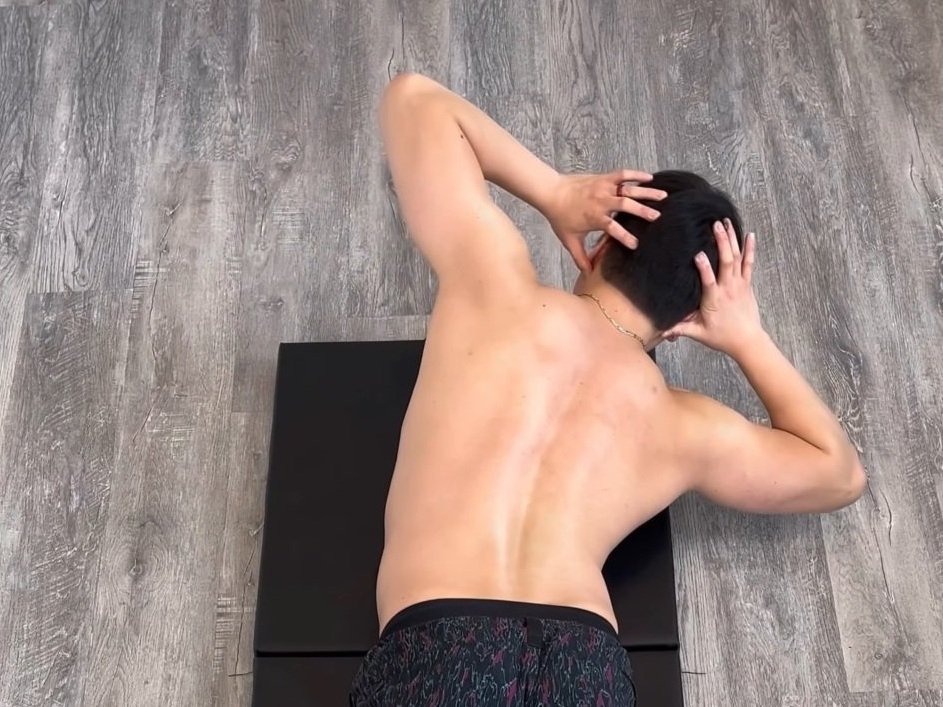
Strength and conditioning the body is used to improve functional independence in patients with transverse myelitis. While exercise rehabilitation is unable to reverse the neurological damage caused by this condition, it can help patients optimize their ability to move independently as possible. Long term rehabilitation is beneficial for improving quality of life, even many years after the acute transverse myelitis episode.
Physical rehabilitation can be provided by exercise specialists including physiotherapists, chiropractors, and naturopaths.
Physiotherapy is used to maintain muscular function, endurance, strength, and coordination. A full body exercise program is used to strengthen movements required in modified activities of daily living. Exercises may require the use of exercise equipment but can be modified to use minimal amounts depending on a patient’s access to exercise facilities.
Pelvic health physiotherapy is used to reduce pelvic floor spasticity and to improve bladder and bowel function.
Chiropractic is just to help maintain joint range of motion, joint mobility, and reduce muscle spasticity. Exercise prescription is used to teach patients how to maintain their flexibility and how to manage their own muscle stiffness.
Adjunct therapies such as acupuncture, or massage therapy can be used to reduce muscle pain or aches that is secondary to the decreased levels of physical activity that may be experienced with patients that have transverse myelitis. These therapies are used to manage symptoms and to improve soft tissue mobility.
To get started with a Rehab Hero chiropractor, physiotherapist, or pelvic health physiotherapist click the button below.
What are the differential diagnosis of transverse myelitis?
Differential diagnosis must include viral myelitis, multiple sclerosis, acute disseminated encephalomyelitis, neuromyelitis optica, vasculitis, ischemia, hematomyelia and spinal arteriovenous malformation; multiple sclerosis and vasculitis are most often found. It is recommended to consult with your primary care health practitioner to rule in or out these differential diagnosis. Referral to a neurologist and/or rheumatologist may be required to confirm your diagnosis.
What is myelomalacia?
Myelomalacia of the spine is a medical condition that occurs when the spinal cord begins to soften. This softening can lead to a loss of spinal cord volume. Myelomalacia occurs when hemorrhaging happens within the spine, or when something halts the flow of blood to the spinal cord. This results in “softening” of the spinal cord itself. Typically, this is caused by an acute injury such as a car accident for example, but it can also happen due to degeneration of the spine over time.
Here are some of the signs and symptoms that may indicate a diagnosis of myelomalacia:
Pain along the spine
Paralysis or any loss of feeling in the legs or arms
Functional loss in any body part
What is cervical spondylotic myelopathy?
What is the relevance to cervical spondylotic myelopathy? Cervical spondylotic myelopathy or CSM for short, is a condition that affects the upper cervical spine. Typical symptoms of CSM include but are not limited to:
sensory changes in the upper limbs such as tingling or numbness
difficulty with hand motions that require dexterity (such as buttoning up a shirt)
weakness in the shoulders, hands, and arms
loss of fine motor skills in the hands
stiffness or pain in the neck
CSM can cause myelomalacia. Before spinal cord volume loss can be seen, early signs of oedema can be detected by the MRI. Therefore, the presence of oedema in CSM is often considered a critical finding in diagnosing myelomalacia.
Written by: Dr. Angeline Foote
‘Dr. Angie’ is a chiropractor that practices in Markham, Ontario. During her appointments she focuses on educating her patients on the root cause of their pain. Outside of the clinic you can find her rock climbing, taking exercise classes, and spending time with her friends and family.