Lipid-Lowering Efficacy of Kuding Tea in Patients With Metabolic Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
- 1Department of Cardiology, Xiyuan Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 2National Clinical Research Center for Chinese Medicine Cardiology, Beijing, China
- 3Academy of Integrative Medicine, Fujian University of Traditional Chinese Medicine, Fuzhou, China
- 4Fujian Key Laboratory of Integrative Medicine on Geriatrics, Fujian University of Traditional Chinese Medicine, Fuzhou, China
Background: Kuding tea (KT), traditional tea material and widely used in China, has been found to have lipid-lowering effect in clinical and experimental studies. However, there has been no systematic review of the evidence on this subject.
Methods: Eight electronic databases were searched from database inception until September 2021 for relevant randomized controlled trials (RCTs). We used the Cochrane Reviewer’s Handbook to assess the quality of the included studies. Weighted mean difference (WMD) and 95% confidence interval (CI) were used to measure the pooled effect size by random-effects model. Funnel plot, Egger regression test, and the Begg’s test was used to assess publication bias.
Results: Eight RCTs involving 716 patients were included in our meta-analysis. Comparing with the control group, KT group reduced serum total cholesterol (TC) levels (WMD: −0.56 mmol/L; 95% CI: −0.64, −0.47; I2 = 56.56%; P = 0.00), triglyceride (TG) levels (WMD: −0.30 mmol/L; 95% CI: −0.35, −0.24; I2 = 88.60%; P = 0.00), and low-density lipoprotein cholesterol (LDL-C) levels (WMD: −0.29 mmol/L; 95% CI: −0.37, −0.21; I2 = 89.43%; P = 0.00), but no significant effects on high-density lipoprotein cholesterol (HDL-C) (WMD: 0.07 mmol/L; 95% CI: −0.02, 0.16; I2 = 93.92%; P = 0.12). The results of sensitivity analysis were not altered after removing each study in turn. Subgroup analyses showed that KT intervention period was the source of heterogeneity. Following analysis, results revealed that long-term (>4 weeks and ≤8 weeks) use of KT increased HDL-C levels (WMD: 0.19; 95% CI: 0.13, 0.25). In addition, both the sensitivity analysis and subgroup analysis showed that our results were robust. No potentially significant publication bias was found from the funnel plot, Begg-Mazumdar correlation test and Egger regression test.
Conclusion: KT supplementation can effectively improve lipid profile and KT is a promising approach to reduce blood lipid level in patients with metabolic disorders.
Systematic Review Registration: [www.crd.york.ac.uk/prospero], identifier [CRD42020221850].
Introduction
Metabolic disorders are multiple risk factor for cardiovascular disease (CVD), including dyslipidemia, obesity (particularly central adiposity), insulin resistance and elevated blood pressure (BP) (1, 2). It is estimated that more than 1 billion people worldwide are affected with metabolic disorders (2), and patients with metabolic disorders are twice as susceptible to develop CVD in the next 5–10 years as non-metabolic disorders patients (3). Clinical trials of therapies lowering lipids [e.g., Low-density lipoprotein cholesterol (LDL-C) and triglyceride (TG)] have consistently shown to reduce the risk of cardiovascular (CV) events (4–9). Lifestyle modifications (such as exercise and diet) can help patients preclude or reduce total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), LDL-C, and TG levels (6, 9). The use of alternative therapies, especially natural medicines and dietary supplements, in the treatment of metabolic disorders has rapidly increased and received increasing attention worldwide over the recent decade (10, 11).
Kuding tea (KT) has a total of 12 species belonging to six families and six genera (12, 13), is a traditional Chinese herb beverage commonly consumed in China, which has been reported to have many health benefits, such as anti-obesity (14), anti-inflammatory (15), anti-oxidation (16), modulating gut microbiota (17), and lowering lipid levels (18). Previous animal studies have shown that kudingcha dicaffeoylquinic acids (diCQAs) reduced the liver and adipose tissue mass, serum TC and LDL-C concentrations in high-fat diet fed mice (19); however, despite numerous randomized controlled trials (RCTs) on the effect of KT on lipid levels, as of yet no systematic review and meta-analysis of these evidence, so we conducted a systematic review and meta-analysis of RCTs involve the KT supplementation in the regulation of lipids.
Methods
Search Strategy
The meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines for RCTs (20) and registered with International Prospective Register of Systematic Reviews (PROSPERO) (registration number: CRD42020221850).1 We searched the PubMed, EMBASE, MEDLINE, Cochrane Library, the Cochrane Central Register of Controlled Trials, China National Knowledge Infrastructure Database (CNKI), Wanfang, and VIP from the inception dates to September 2021 for RCTs, without language restrictions. Two reviewers screened through the above electronic databases. Supplementary Appendix A shows the detailed search strategies. We obtained additional articles of research expertise in lipids from domain expert, and searched for additional studies from a list of references, related studies, and reviews of studies identified in a literature search.
Selection Criteria
We screened the selected studies in strict accordance with the principles of PICOS (Participants, Interventions, Comparisons, Outcomes, and Study design).
Participants: Patients with metabolic disorders were diagnosed according to recognized diagnostic criteria (IFD, WHO, or NCEP-ATP III) (3).
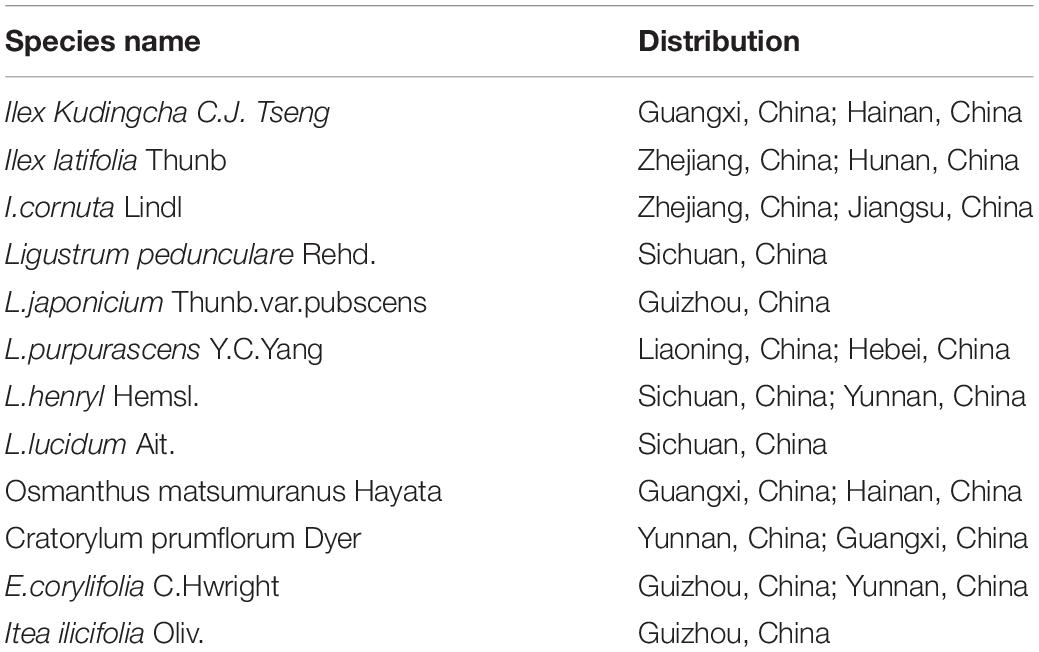
Interventions: Supplement KT or related supplements. The species name and distribution of KT are shown in Table 1 (12, 13).
Comparison: No use of KT or KT-related supplements categories of exposure.
Outcome: Lipid parameters (TC, TG, HDL-C and LDL-C).
Study design: Randomized controlled trials (RCTs).
Data Extraction and Quality Assessment
Two reviewers independently extracted the following information from each study using a standardized electronic form: first author, publication year, country, sample characteristics, study design, dose of KT, duration, baseline serum TC, TG, HDL-C, LDL-C concentration and other information including age and sex. Disagreements were resolved by consulting with a third investigator.
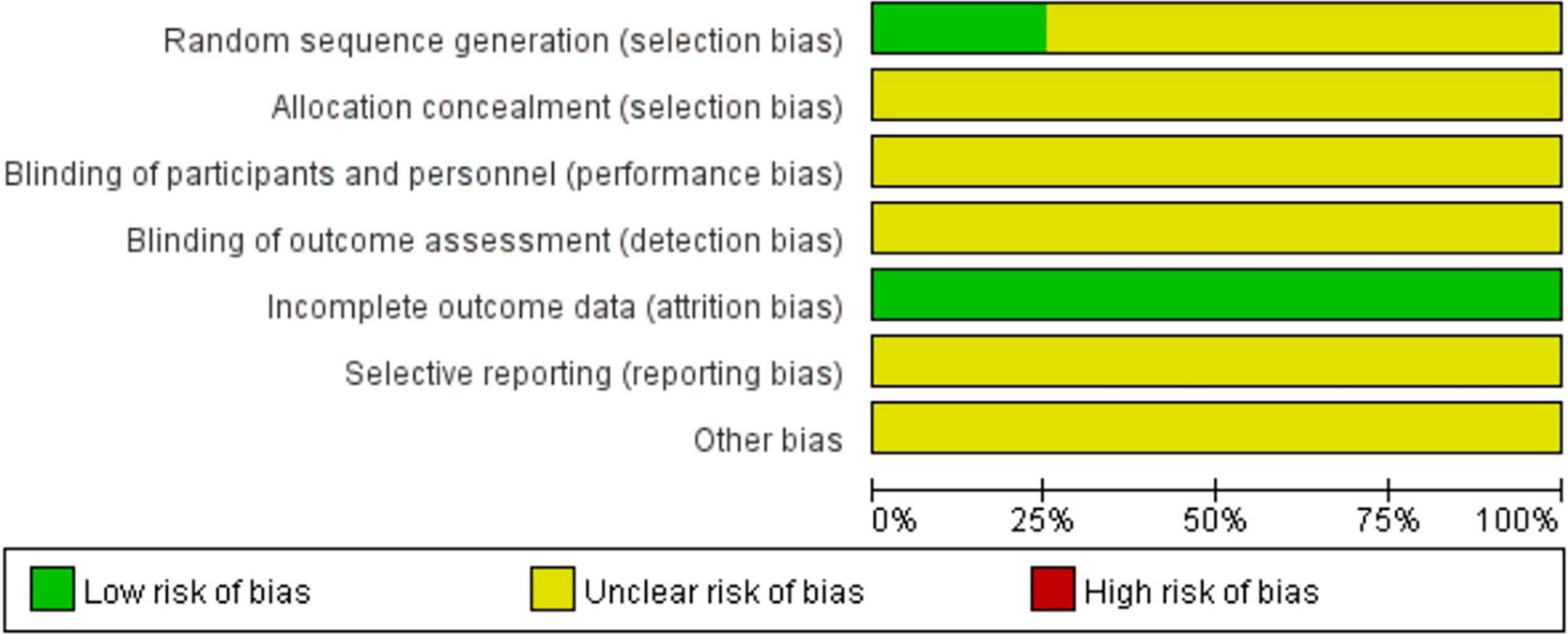
We used the Cochrane Collaboration risk of Bias Tool to assess the quality of the included studies in the following seven domains: the generation of random sequences, allocation concealment, blinded method used, integrity of the outcome data, selective outcome reporting, and other bias. Based on information provided by journal publications, we rated the risk of bias for each criterion as low, high, or unclear.
Data Synthesis and Analysis
For statistical analysis, the SD in TC, TG, HDL-C and LDL-C from baseline was used to calculate the mean difference (MD) between the KT group and the control group. The pooled effect size was measured with weighted mean difference (WMD) and 95% confidence interval (CI). Statistical heterogeneity across studies was examined using Cochran’s Q-test (test level α = 0.1) and I2 statistic. The effects of binary and continuous risk factors were estimated using a random-effects model (DerSimonian and Laird method). Sensitivity analysis was conducted to determine the impact of each study on the overall effect size by using leave-one-out method, and subgroup analysis was performed to investigate potential sources of heterogeneity in the trials. Publication bias was assessed by funnel plot, Egger regression test, and the Begg-Mazumdar correlation test. Analyses were performed using Stata (version 16.0) and Review Manager (version 5.3).
Results
Search Results and Study Inclusion
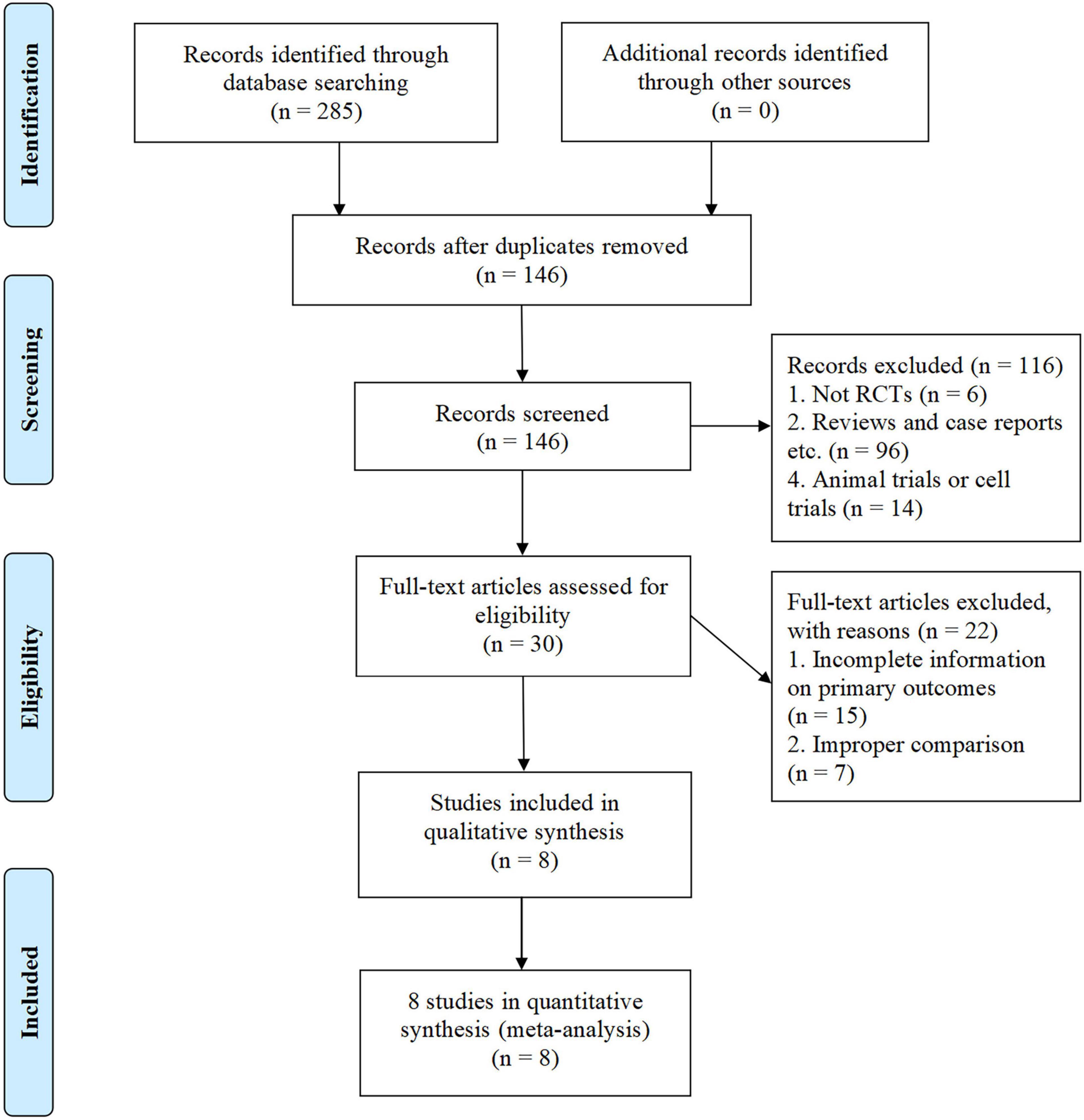
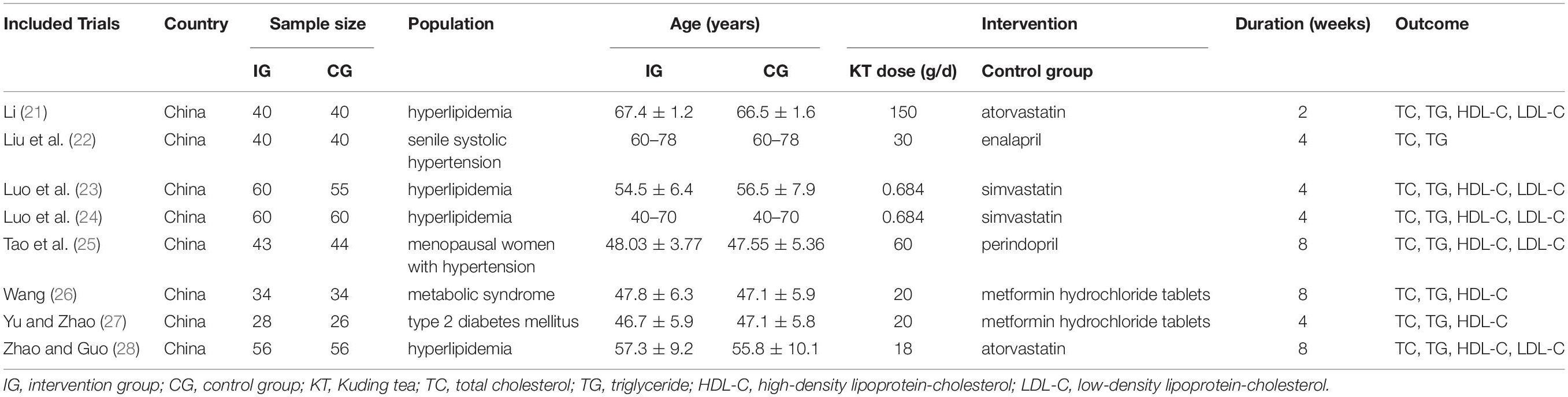
The initial search from PubMed, EMBASE, MEDLINE, Cochrane Library, the Cochrane Central Register of Controlled Trials, CNKI, Wanfang, and VIP databases identified 285 potentially relevant articles for screening, of which 139 were removed due to duplication. The remaining 146 articles were further screened and 116 studies were excluded for the following reasons: study not designed as the RCTs (n = 6); experimental studies (n = 14); reviews and case reports etc. (n = 96). The full text of the remaining 30 articles was further screened, and 22 of them were excluded for the following reasons: incomplete information on primary outcomes (n = 15) and improper comparison (n = 7). Finally, 8 articles entered into our meta-analysis, involving 716 patients (361 [50.4%] in the KT group, 355 [49.6%] in the control group) (Figure 1). All included studies were conducted and published in China (21–28). The average sample size of these trials was about 90 participants (54 to 120 participants per trial). The course of treatment fluctuated between 2 and 8 weeks. The control group of all included studies were conventional western medicine, including atorvastatin (21, 28), simvastatin (23, 24), enalapril (22), perindopril (25), metformin hydrochloride tablets (26, 27). The characteristics of the included studies are shown in Table 2.
Quality Assessment
The quality assessment of the included studies was shown in Figure 2. All of the included studies (21–28) described the random sequence generation methods, among which 2 studies (25, 28) used computer-generated list of random numbers. The rest included studies only mentioned random, did not report it in detail. In addition, selective reporting, allocation concealment and blind were not very clear.
Effects of Kuding Tea on Lipid Levels
Total Cholesterol
Eight studies (21–28) reported the effect of KT supplementation on TC levels (Figure 3A). Compared with the control group, KT group reduced TC levels (WMD: −0.56 mmol/L; 95% CI: −0.64, −0.47; I2 = 56.56%; P = 0.00). Sensitivity analysis showed that the results did not change before and after sensitivity analysis (Figure 4A). Inter-group heterogeneity changed after subgroup analysis based on dose and duration of KT supplementation, and statins/non-statins as control group, but there was no significant difference in TC levels before and after subgroup analysis (Figures 5A–C).
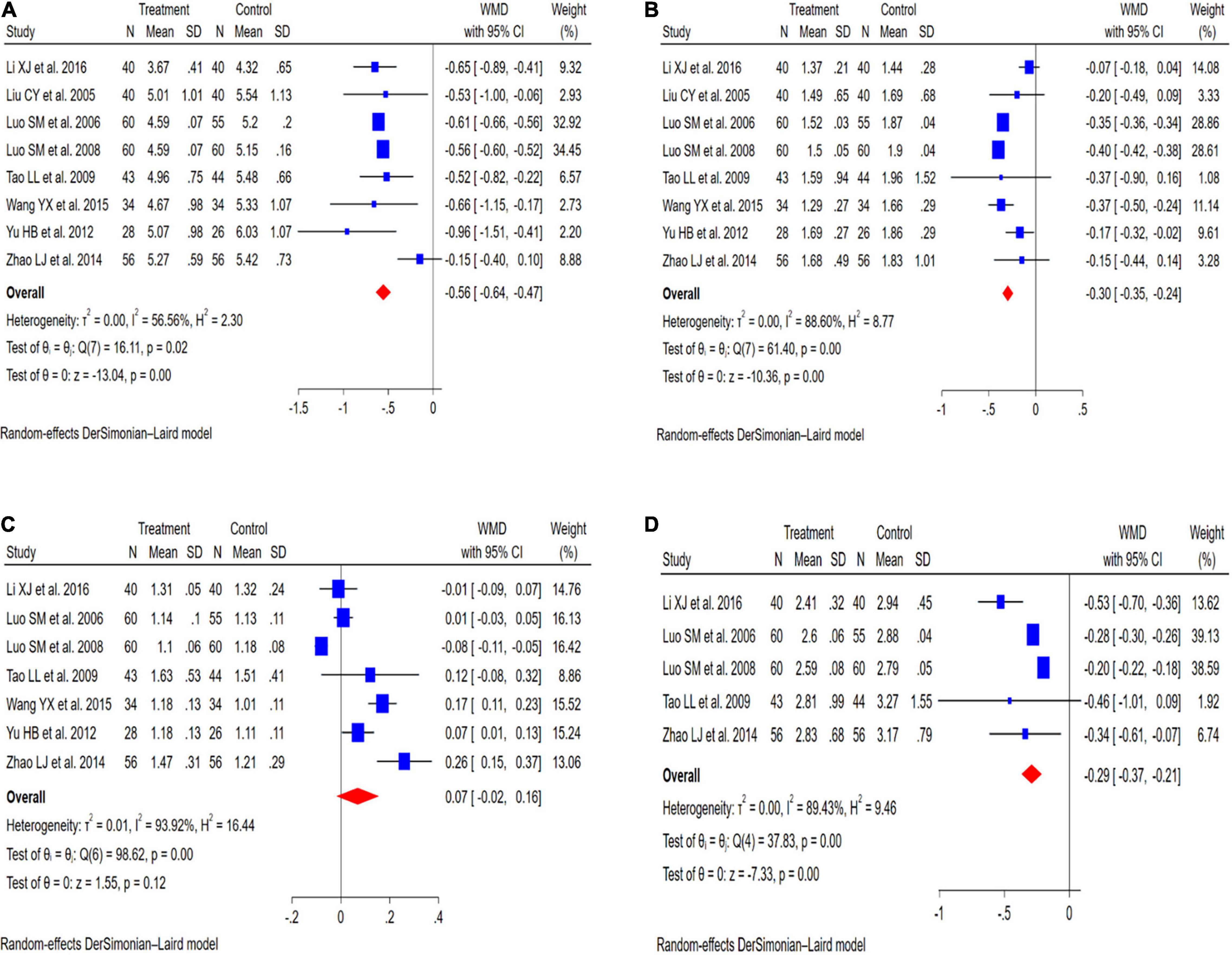
Figure 3. Meta-analysis results of KT supplementation for lipid levels. (A) TC levels. (B) TG levels. (C) HDL-C levels. (D) LDL-C levels.
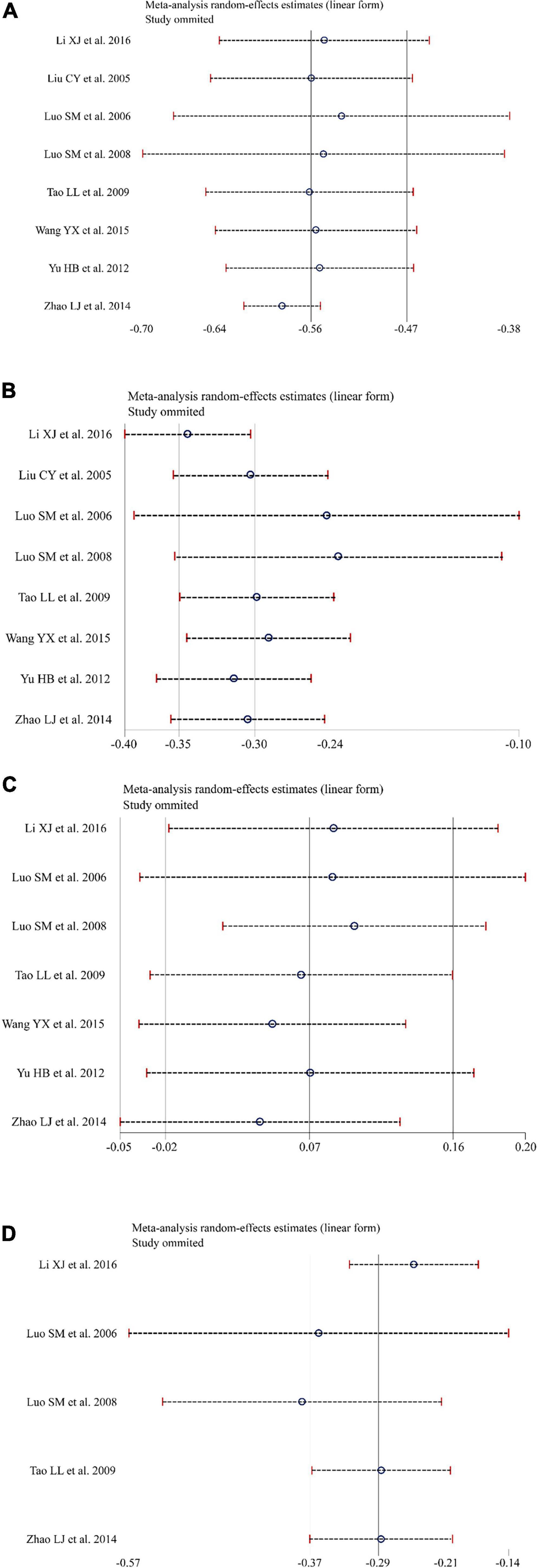
Figure 4. Sensitivity analysis was conducted to determine the impact of each study on the overall effect size by using removing each study in turn. (A) Sensitivity analysis for total cholesterol (TC). (B) Sensitivity analysis for triglyceride (TG). (C) Sensitivity analysis for high-density lipoprotein cholesterol (HDL-C). (D) Sensitivity analysis for low-density lipoprotein cholesterol (LDL-C).
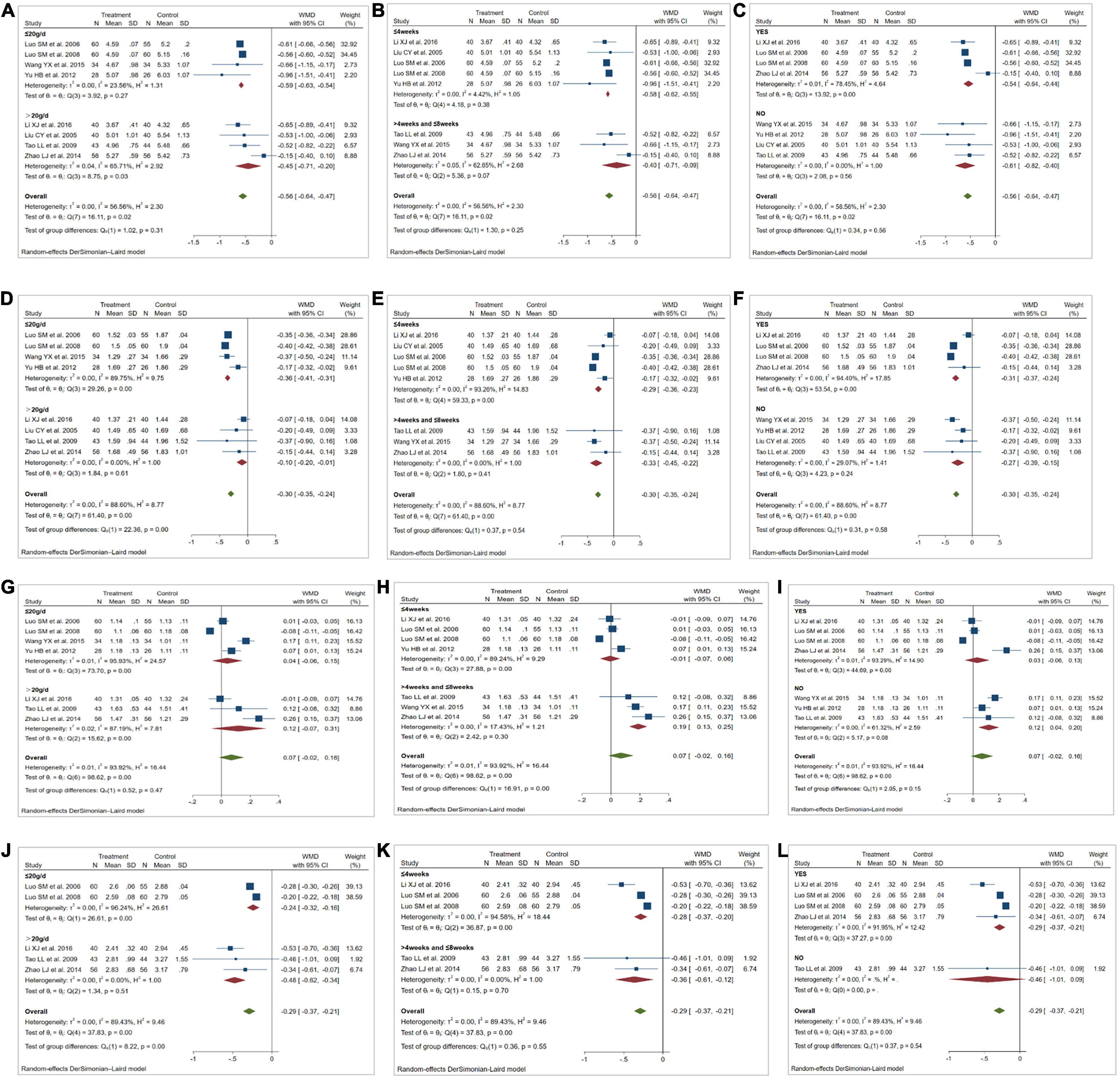
Figure 5. Results of subgroup analysis. (A,D,G,J) Effect of dose of Kuding tea (KT) on total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C). low-density lipoprotein cholesterol (LDL-C). (B,E,H,K) Effect of duration of KT intervention on TC, TG, HDL-C, LDL-C. (C,F,I,L) Effect of KT use and whether statins were used in the control group on TC, TG, HDL-C, LDL-C. WMD, weighted mean difference.
Triglyceride
Eight studies (21–28) evaluated the effect of KT supplementation on TG levels. Our meta-analysis revealed a significant reduction in TG levels following KT supplementation (WMD: −0.30 mmol/L; 95% CI: −0.35, −0.24; I2 = 88.60%; P = 0.00) (Figure 3B). A sensitivity analysis was performed that separately excluded the individual trials, and the results remained unchanged (Figure 4B). The heterogeneity has changed between different intervention time groups, dose and statins/non-statins as control group, but there were no significant differences before and after subgroup analysis (Figures 5D–F).
High-Density Lipoprotein Cholesterol
Effect of KT supplementation on HDL-C levels was investigated in seven trials (21, 23–28). As shown in Figure 3C, there was no statistically significant reduction of KT supplementation on HDL-C levels (WMD: 0.07 mmol/L; 95% CI: −0.02, 0.16; I2 = 93.92%; P = 0.12). The results of sensitivity analysis were not altered after removing each study in turn (Figure 4C). Subgroup analysis suggested that a dose of KT and statins/non-statins as control group had no significant impact on between-study heterogeneity (Figures 5G,I). However, long-term (>4 weeks and ≤8 weeks) use of KT may increase HDL-C levels (WMD: 0.19; 95% CI: 0.13, 0.25) (Figure 5H).
Low-Density Lipoprotein Cholesterol
Forest plots demonstrating the effects of KT supplementation on lipids are shown in Figure 3D. Our meta-analysis of seven studies (21, 23–25, 28) showed that KT supplementation decreased LDL-C (WMD: −0.29 mmol/L; 95% CI: −0.37, −0.21; I2 = 89.43%; P = 0.00). Sensitivity analysis showed no significant change in the overall estimate of effect size after excluding the individual trials (Figure 4D). Subgroup analysis showed no significant differences within subgroups based on the dose of KT, duration of KT supplementation and statins/non-statins as control group on LDL-C levels (Figures 5J–L).
Publication Bias
As shown in Figures 6A–L, funnel plot, Begg–Mazumdar correlation test and Egger regression test were used to evaluate the quality of meta-analysis, no publication bias for TC (Begg–Mazumdar correlation test, Kendall’s score = −6, continuity-corrected z = 0.62, continuity-corrected P = 0.54; Egger regression test, coefficient, 0.21; 95% CI, −1.73 to 2.14; P = 0.80), TG (Begg-Mazumdar correlation test, Kendall’s score = −4, continuity-corrected z = 0.37, continuity-corrected P = 0.71; Egger regression test, coefficient, 1.70; 95% CI, −1.34 to 4.73; P = 0.22), HDL-C (Begg–Mazumdar correlation test, Kendall’s score = 5, continuity-corrected z = 0.60, continuity-corrected P = 0.55; Egger regression test, coefficient, 5.41; 95% CI, −0.27 to 11.08; P = 0.06), and LDL-C (Begg–Mazumdar correlation test, Kendall’s score = 2, continuity-corrected z = 0.24, continuity-corrected P = 0.81; Egger regression test, coefficient, −1.24; 95% CI, −7.95 to 5.47; P = 0.60).
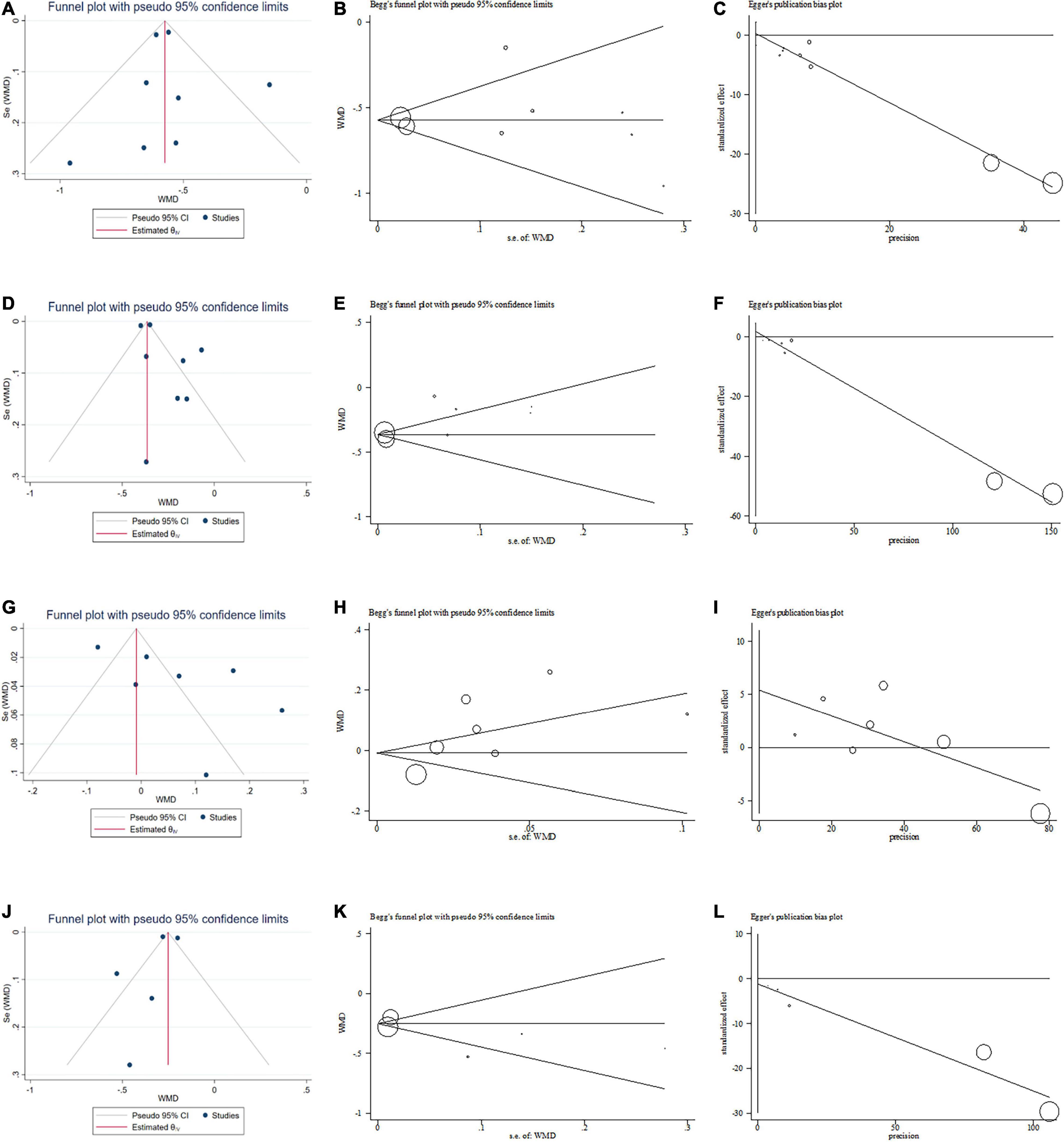
Figure 6. Publication bias. (A) Funnel plot for total cholesterol (TC). (B) Begg test for TC. (C) Egger test for TC. (D) Funnel plot for triglyceride (TG). (E) Begg test for TG. (F) Egger test for TG. (G) Funnel plot for high-density lipoprotein cholesterol (HDL-C). (H) Begg test for HDL-C. (I) Egger test for HDL-C. (J) Funnel plot for low-density lipoprotein cholesterol (LDL-C). (K) Begg test for LDL-C. (L) Egger test for LDL-C. WMD, weighted mean difference.
Discussion
To our knowledge, this is the first meta-analysis to evaluate the effects of KT on lipid levels. This systematic analysis included eight RCTs involving 716 patients (361 in the KT group, 355 in the control group) of KT supplementation interventions for lipid levels and identified evidence of their beneficial effects on reducing serum TC, TG, and LDL-C levels. Subgroup analysis results showed that long-term (>4 weeks and ≤8 weeks) use of KT may increase HDL-C levels. In addition, both the sensitivity analysis and subgroup analysis showed that our results were robust.
Previous meta-analyses have shown that lowering TC levels, especially regimens that reduce LDL-C by about 1.5 mmol/L, not only reduce the incidence of ischemic heart disease (IHD), but also reduce by about a third the incidence of ischemic stroke, regardless of age, blood pressure, or or prerandomisation blood lipid concentrations (29, 30). In addition, studies have shown that the reduction of non-HDL-C by 1 mmol/L, the increase of HDL-C by 0.33 mmol/L and the decrease of total/HDL-C by 1.33 can reduce the mortality of IHD by about a third (30), while the decrease of TG by 0.1 mmol/L can reduce coronary events by 5% (31, 32). The weighted mean reductions in TC, TG and LDL-C appearing due to KT supplementation as observed in the present study (TC: 0.56 mmol/L; TG: 0.30 mmol/L; LDL-C: 0.29 mmol/L), may be important for the primary prevention of dyslipidemia. Moreover, KT has the advantages of low price (0.02–0.07 USD a day) and easy availability.
There are various mechanisms involved in the regulation of blood lipid levels by KT supplementation. It is suggested that KT extracts can modulate lipid metabolism disorders, upregulated mRNA expressions of peroxisome proliferator-activated receptor-α (PPAR-α), carnitine palmitoyltransferase-I (CPT-1), lipoprotein lipase (LPL), and cholesterol 7 alpha hydroxylase (CYP7A1) and downregulated mRNA expressions of peroxisome proliferator-activated receptor-γ (PPAR-γ) and CCAAT/enhancer-binding protein-alpha (C/EBP-α), which reduced adipocyte differentiation and lipid accumulation and improved dyslipidemia (33–36). In accordance with our results, several animal studies have reported that KT or its bioactive compounds significantly improved plasma lipid parameters, including TC, TG, and LDL-C (37–39). Moreover, it has also been confirmed that KT-derived saponins increased the content of serum lysoglycerophospholipids (Lyso-GPLs) and thus have a positive effect on lipid metabolism (40).
This meta-analysis has several limitations. First, heterogeneity of included studies was the most important limitation of this meta-analysis. Sensitivity analysis and subgroup analysis were conducted to analyze the factors (dose, duration, etc.) that may lead to considerable heterogeneity and explore the sources of heterogeneity. Heterogeneity changed after analysis, but the overall results were robust. Second, since all the studies were conducted in China, we cannot demonstrate whether the results can be stable in other parts of the world, and we cannot clarify the impact of differences in race, region and socio-economic characteristics on the results. In addition, the quality of some RCTs is poor, for example, unclear allocation concealment and blind method, although we adopt strict literature quality evaluation criteria.
The current available evidence to support the widespread use of KT is still limited and deserves additional attention, and KT supplements should never replace statins or other pharmacological approaches to reducing blood lipid levels as an adjuvant treatment strategy to effectively improve dyslipidemia and reduce the risk of CVD, especially in patients with statin intolerance and low to medium grade of dyslipidemia.
Conclusion
This meta-analysis showed that KT supplementation seemed to improve metabolic disorders, and KT supplementation could reduce TC, TG, and LDL-C levels. The study also showed that long-term (>4 weeks and ≤8 weeks) supplementation of KT may increase HDL-C levels. This potential benefit needs to be further assessed through more rigorous and large-scale RCTs. Furthermore, this study provides useful information for the effect of KT on lipids and provides a way for the application of new lipid control therapies.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author Contributions
ZJ designed the research and wrote the initial draft. ZJ, ZL, TW, and YW analyzed and synthesized the study data. JC, KC, and ZG managed and coordinated the responsibility for the research. All authors contributed to the article and approved the submitted version.
Funding
This work was financially supported by the National Science and Technology Major Project of the Ministry of Science and Technology of China (2019ZX09201005-002-006), and the Beijing Traditional Chinese Medicine Science and Technology Development Fund Project (JJ-2020-79).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.802687/full#supplementary-material
Footnotes
References
1. Grundy SM, Brewer HBJr, Cleeman JI, Smith SCJr, Lenfant C American Heart Association, et al. Definition of metabolic syndrome: report of the national heart, lung, and blood institute/American heart association conference on scientific issues related to definition. Circulation. (2004) 109:433–8. doi: 10.1161/01.cir.0000111245.75752.c6
2. Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. (2018) 20:12. doi: 10.1007/s11906-018-0812-z
3. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: a joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation. (2009) 120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644
4. Gencer B, Marston NA, Im K, Cannon CP, Sever P, Keech A, et al. Efficacy and safety of lowering LDL cholesterol in older patients: a systematic review and meta-analysis of randomised controlled trials. Lancet. (2020) 396:1637–43. doi: 10.1016/S0140-6736(20)32332-1
5. Sabatine MS, Wiviott SD, Im K, Murphy SA, Giugliano RP. Efficacy and safety of further lowering of low-density lipoprotein cholesterol in patients starting with very low levels: a meta-analysis. JAMA Cardiol. (2018) 3:823–8. doi: 10.1001/jamacardio.2018.2258
6. Kopin L, Lowenstein C. Dyslipidemia. Ann Intern Med. (2017) 167:ITC81–96. doi: 10.7326/AITC201712050
7. Anderson KM, Castelli WP, Levy D. Cholesterol and mortality. 30 years of follow-up from the Framingham study. JAMA. (1987) 257:2176–80. doi: 10.1001/jama.257.16.2176
8. Goldbourt U, Yaari S. Cholesterol and coronary heart disease mortality. A 23-year follow-up study of 9902 men in Israel. Arteriosclerosis. (1990) 10:512–9. doi: 10.1161/01.atv.10.4.512
9. Wilkins JT, Lloyd-Jones DM. Novel lipid-lowering therapies to reduce cardiovascular risk. JAMA. (2021) 326:266–7. doi: 10.1001/jama.2021.2244
10. Bahmani M, Mirhoseini M, Shirzad H, Sedighi M, Shahinfard N, Rafieian-Kopaei M. A review on promising natural agents effective on hyperlipidemia. J Evid Based Complement Altern Med. (2015) 20:228–38. doi: 10.1177/2156587214568457
11. Liu ZL, Li GQ, Bensoussan A, Kiat H, Chan K, Liu JP. Chinese herbal medicines for hypertriglyceridaemia. Cochrane Database Syst Rev. (2013) CD009560. doi: 10.1002/14651858.CD009560.pub2
12. He ZD, Lau KM, But PP, Jiang RW, Dong H, Ma SC, et al. Antioxidative glycosides from the leaves of Ligustrum robustum. J Nat Prod. (2003) 66:851–4. doi: 10.1021/np020568g
13. Wüpper S, Lüersen K, Rimbach G. Chemical composition, bioactivity and safety aspects of kuding tea-from beverage to herbal extract. Nutrients. (2020) 12:2796. doi: 10.3390/nu12092796
14. Chen G, Xie M, Dai Z, Wan P, Ye H, Zeng X, et al. Kudingcha and fuzhuan brick tea prevent obesity and modulate gut microbiota in high-fat diet fed mice. Mol Nutr Food Res. (2018) 62:e1700485. doi: 10.1002/mnfr.201700485
15. Hu T, He XW, Jiang JG. Functional analyses on antioxidant, anti-inflammatory, and antiproliferative effects of extracts and compounds from Ilex latifolia Thunb., a Chinese bitter tea. J Agric Food Chem. (2014) 62:8608–15. doi: 10.1021/jf501670v
16. Fan J, Wu Z, Zhao T, Sun Y, Ye H, Xu R, et al. Characterization, antioxidant and hepatoprotective activities of polysaccharides from Ilex latifolia Thunb. Carbohydr Polym. (2014) 101:990–7. doi: 10.1016/j.carbpol.2013.10.037
17. Wan P, Peng Y, Chen G, Xie M, Dai Z, Huang K, et al. Modulation of gut microbiota by Ilex kudingcha improves dextran sulfate sodium-induced colitis. Food Res Int. (2019) 126:108595. doi: 10.1016/j.foodres.2019.108595
18. Feng RB, Fan CL, Liu Q, Liu Z, Zhang W, Li YL, et al. Crude triterpenoid saponins from Ilex latifolia (Da Ye Dong Qing) ameliorate lipid accumulation by inhibiting SREBP expression via activation of AMPK in a non-alcoholic fatty liver disease model. Chin Med. (2015) 10:23. doi: 10.1186/s13020-015-0054-9
19. Xie M, Chen G, Wan P, Dai Z, Zeng X, Sun Y. Effects of dicaffeoylquinic acids from Ilex kudingcha on lipid metabolism and intestinal microbiota in high-fat-diet-fed mice. J Agric Food Chem. (2019) 67:171–83. doi: 10.1021/acs.jafc.8b05444
20. Moher D, Liberati A, Tetzlaff J, Altman DG Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535.
21. Li XJ. Lipid-lowering mechanism of total terpenoids from kudingcha. Guidel Health Care. (2016) 24:286.
22. Liu CY, Yu ZQ, Cao XY. Observation on curative effect of Huxin Jiangya Decoction II on 40 cases of senile systolic hypertension. Hebei J Tradit Chin Med. (2005) 11:819+864.
23. Luo SM, Xin ZJ, Li HB. Observation of therapeutic effect of Jiangzhi tea on 60 cases of hyperlipidemia. Guid J Tradit Chin Med Pharm. (2006) 09:27–8.
24. Luo SM, Chen ZH, Chen NG, Zhou ZW, Xin ZJ, Li HB. Observation on 60 cases of hyperlipidemia treated by Jiangzhi tea combined with simvastatin. Zhejiang J Integr Tradit Chin West Med. (2008) 18:740–1.
25. Tao LL, Ma XC, Chen KJ. Clinical study on effect of Qingxuan Tiaoya recipe in treating menopausal women with hypertension. Chin J Integr Tradit West Med. (2009) 29:680–4.
26. Wang YX. Clinical study on the treatment of metabolic syndrome by Kudingcha Holly. Lishizhen Med Mater Med Res. (2015) 26:914–6.
27. Yu HB, Zhao D. Clinical study on the effects of Kudingcha on blood glucose, lipids and hemorheology in patients with type 2 diabetes mellitus. China Pharm. (2012) 15:1758–60.
28. Zhao LJ, Guo Y. Clinical research of Ziyin Ditan Tiaozhi prescription combined with atorvastatin in the treatment of primary hyperlipidemia. J Chin Med. (2014) 29:1661–3.
29. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. (2005) 366:1267–78. doi: 10.1016/S0140-6736(05)67394-1
30. Prospective Studies Collaboration, Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. (2007) 370:1829–39. doi: 10.1016/S0140-6736(07)61778-4
31. Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. (2014) 384:626–35. doi: 10.1016/S0140-6736(14)61177-6
32. Jun M, Foote C, Lv J, Neal B, Patel A, Nicholls SJ, et al. Effects of fibrates on cardiovascular outcomes: a systematic review and meta-analysis. Lancet. (2010) 375:1875–84. doi: 10.1016/S0140-6736(10)60656-3
33. Wu H, Chen YL, Yu Y, Zang J, Wu Y, He Z. Ilex latifolia Thunb protects mice from HFD-induced body weight gain. Sci Rep. (2017) 7:14660. doi: 10.1038/s41598-017-15292-x
34. Wu Y, Yang J, Liu X, Zhang Y, Lei A, Yi R, et al. Preventive effect of small-leaved kuding tea (Ligustrum robustum) on high-diet-induced obesity in C57BL/6J mice. Food Sci Nutr. (2020) 8:4512–22. doi: 10.1002/fsn3.1758
35. Kang SU, Kim HJ, Kim DH, Han CH, Lee YS, Kim CH. Nonthermal plasma treated solution inhibits adipocyte differentiation and lipogenesis in 3T3-L1 preadipocytes via ER stress signal suppression. Sci Rep. (2018) 8:2277. doi: 10.1038/s41598-018-20768-5
36. Mueller E, Drori S, Aiyer A, Yie J, Sarraf P, Chen H, et al. Genetic analysis of adipogenesis through peroxisome proliferator-activated receptor gamma isoforms. J Biol Chem. (2002) 277:41925–30. doi: 10.1074/jbc.M206950200
37. Fan S, Zhang Y, Hu N, Sun Q, Ding X, Li G, et al. Extract of kuding tea prevents high-fat diet-induced metabolic disorders in C57BL/6 mice via liver X receptor (LXR) β antagonism. PLoS One. (2012) 7:e51007. doi: 10.1371/journal.pone.0051007
38. Xie M, Dai Z, Wan P, Ye H, Zeng X, Sun Y. Kudingcha and Fuzhuan brick tea prevent obesity and modulate gut microbiota in high-fat diet fed mice. Mol Nutr Food Res. (2018) 62:e1700485. doi: 10.1002/mnfr.201700485
39. Song C, Yu Q, Li X, Jin S, Li S, Zhang Y, et al. The hypolipidemic effect of total saponins from kuding tea in high-fat diet-induced hyperlipidemic mice and its composition characterized by UPLC-QTOF-MS/MS. J Food Sci. (2016) 81:H1313–9. doi: 10.1111/1750-3841.13299
Keywords: kuding tea (KT), lipid profile, systematic review, meta-analysis, metabolic disorders
Citation: Jiang Z, Lu Z, Wang T, Wang Y, Chu J, Chen K and Gao Z (2022) Lipid-Lowering Efficacy of Kuding Tea in Patients With Metabolic Disorders: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Nutr. 9:802687. doi: 10.3389/fnut.2022.802687
Received: 27 October 2021; Accepted: 18 March 2022;
Published: 28 April 2022.
Edited by:
Ozra Tabatabaei-Malazy, Tehran University of Medical Sciences, IranReviewed by:
Devina Adella, University of Pelita Harapan, IndonesiaBunleu Sungthong, Mahasarakham University, Thailand
Copyright © 2022 Jiang, Lu, Wang, Wang, Chu, Chen and Gao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jianfeng Chu, jianfengchu@126.com; Keji Chen, kjchenvip@163.com; Zhuye Gao, zhuyegao2021@163.com
 Zhonghui Jiang
Zhonghui Jiang Zhuqing Lu3,4
Zhuqing Lu3,4  Jianfeng Chu
Jianfeng Chu