Abstract
Purpose of Review
Pityriasis versicolor (PV) is a superficial mycosis that it can occur at any age, even in newborns. In this review, we will describe epidemiological data, mycological characteristics of yeast, pathogenesis and clinical characteristics of the disease, different diagnostic resources, and the current recommendations for treatment.
Recent Findings
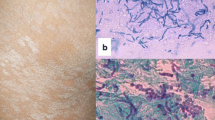
The typical morphology and topography of PV allow us to make a quick diagnosis, but atypical presentations have been described. Diagnostic tools, such as dermoscopy, can also reveal patterns that allow the evaluation of characteristics of scales and pigment in lesions. The discovery of new species and new mechanisms of interaction with the host has broadened the panorama of aetiological possibilities.
Summary
Although PV is a common disorder, extensive research is necessary to better understand the pathophysiology of the disease, immunological characteristics of the pathogen-host relationship and resources needed to precisely diagnose the disease, treat the disease, and avoid its chronic and recurrent course.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Heidrich D, Daboit TC, Stopiglia CDO, Magagnin CM, et al. Sixteen years of pityriasis versicolor in metropolitan area of Porto Alegre, Southern Brazil. Rev. Inst. Med. Trop. 2015;57:277–80. https://doi.org/10.1590/S0036-46652015000400001This article presents the study with the highest number of patients.
Negroni R. Historical aspects of dermatomycoses. Clin Dermatol. 2010;28:125–32. https://doi.org/10.1016/j.clindermatol.2009.12.010.
Ashbee HR, Evans EGV. Immunology of diseases associated with Malassezia species. Clin Microbiol Rev. 2002;15:21–57. https://doi.org/10.1128/CMR.15.1.21.
Theelen B, Cafarchia C, Gaitanis G, Bassukas ID, et al. Malassezia ecology, pathophysiology, and treatment. Med Mycol. 2018;56:S10–25. https://doi.org/10.1093/mmy/myx134.
Hellgren L, Vincent J. The incidence of tinea versicolor in central Sweden. J Med Microbiol. 1983;16:501–2. https://doi.org/10.1099/00222615-16-4-501.
Gupta A, Bluhm R, Summerbell R. Pityriasis versicolor. J Eur Acad Dermatol Venereol. 2002;16:19–33.
Wyre HW, Johson T. Neonatal pityriasis versicolor. Arch Dermatol. 1981;117:752–3.
Congly H. Pityriasis versicolor in a 3-month-old boy. Can Med Assoc J. 1984;130:844–5.
Oliveira-Santana J, Costa-Campos-Filho P, Andrade-De Azevedo LF. Pityriasis versicolor: clinical-epidemiological characterization of patients in the urban area of Buerarema-BA. Brazil. An Bras Dermatol. 2013;88:216–21. https://doi.org/10.1590/S0365-05962013000200005.
Sharma A, Rabha A, Choraria S, Hazarika D, et al. Clinicomycological profile of pityriasis versicolor in Assam. Indian J Pathol Microbiol. 2016;59:159–65. https://doi.org/10.4103/0377-4929.182027.
Alvarado Z, Pereira C. Fungal diseases in children and adolescents in a referral centre in Bogota. Colombia. Mycoses. 2018;61:543–8. https://doi.org/10.1111/myc.12774.
Ferie J, Dinkela A, Mbata M, Idindili B, et al. Skin disorders among school children in rural Tanzania and an assessment of therapeutic needs. Trop Doct. 2006;36:219–21. https://doi.org/10.1258/004947506778604823.
Kumar-Jena D, Sengupta S, Chandra-Dwari B, Kumar-Ram M. Pityriasis versicolor in the pediatric age group. Indian J Dermatol Venereol Leprol. 2005;71:259–61. https://doi.org/10.4103/0378-6323.16618.
Silva-Rocha WP, De Azevedo MF, Chaves GM. Epidemiology and fungal species distribution of superficial mycoses in Northeast Brazil. J Mycol Med. 2017;27:57–64. https://doi.org/10.1016/j.mycmed.2016.08.009.
Yahya H. Knowledge, perception, and practice of patients about pityriasis versicolor in Kaduna. North Central Nigeria. Int J Dermatol. 2017;56:1169–74. https://doi.org/10.1111/ijd.13654.
Aljabre SHM, Alzayir AAA, Abdulghani M, Osman OO. Pigmentary changes of tinea versicolor in dark-skinned patients. Int J Dermatol. 2001;40(4):273–5. https://doi.org/10.1046/j.1365-4362.2001.01201.x.
Rodoplu G, Saracli MA, Gümral R, Yildiran ST. Distribution of Malassezia species in patients with pityriasis versicolor in Turkey. J Mycol Med. 2014;24:117–23. https://doi.org/10.1016/j.mycmed.2014.02.001.
Xie Z, Ran Y, Zhang H, Zhang M, et al. An analysis of the Malassezia species distribution in the skin of patients with pityriasis versicolor in Chengdu. China. Sci. World J. 2014. https://doi.org/10.1155/2014/182596.
Ibekwe PU, Ogunbiyi AO, Besch R, Ruzicka T, et al. The spectrum of Malassezia species isolated from students with pityriasis vesicolor in Nigeria. Mycoses. 2015;58:203–8. https://doi.org/10.1111/myc.12298.
Moallaei H, Namazi MJ, Bouchara JP, Pourhammed S. Malassezia species in students from universities of Sabzevar. Northeastern Iran. J Mycol Med. 2018;28:70–5. https://doi.org/10.1016/j.mycmed.2017.12.004.
Elshabrawy WO, Saudy N, Sallam M. Molecular and phenotypic identification and speciation of Malassezia yeasts isolated from Egyptian patients with pityriasis versicolor. J Clin Diagn Res. 2017;11:DC12–7. https://doi.org/10.7860/JCDR/2017/27747.10416.
Diongue K, Kébé O, Faye MD, Samb D, et al. MALDI-TOF MS identification of Malassezia species isolated from patients with pityriasis versicolor at the seafarers’ medical service in Dakar. Senegal. J Mycol Med. 2018;28:590–3. https://doi.org/10.1016/j.mycmed.2018.09.007.
Honnavar P, Ghosh AK, Paul S, Shankarnarayan SA, et al. Identification of Malassezia species by MALDI-TOF MS after expansion of database. Diagn Microbiol Infect Dis. 2018;92:118–23. https://doi.org/10.1016/j.diagmicrobio.2018.05.015.
Cam VT, Van TN, Hau KT, Huu DL, et al. Distribution of Malassezia species from scales of patient with pityriasis versicolor by culture in Vietnam. Open Access Maced J Med Sci. 2019;7:184–6. https://doi.org/10.3889/oamjms.2019.091.
Awad AK, Al-Ezzy AIA, Jameel GH. Phenotypic identification and molecular characterization of Malassezia Spp. isolated from pityriasis versicolor patients with special emphasis to risk factors in Diyala Province, Iraq. Open Access Maced J Med Sci. 2019;7. https://doi.org/10.3889/oamjms.2019.128.
Ramadán S, Sortino M, Bulacio L, Marozzi ML, et al. Prevalence of Malassezia species in patients with pityriasis versicolor in Rosario, Argentina. Rev Iberoam Micol. 2012;29:14–9. https://doi.org/10.1016/j.riam.2011.03.001.
Pedrosa AF, Lisboa C, Gonҫalves-Rodrigues A. Malassezia infections: a medical conundrum. J Am Acad Dermatol. 2014;71:170–6. https://doi.org/10.1016/j.jaad.2013.12.022.
Lorch JM, Palmer JM, Vanderwolf KJ, Schmidt KZ, et al. Malassezia vespertilionis sp. nov.: a new cold-tolerant species of yeast isolated from bats. Persoonia. 2018;41:56–70. https://doi.org/10.3767/persoonia.2018.41.04.
Dawson TL. Previews Malassezia : The forbidden kingdom opens. Cell Host Microbe. 2019;25:345–7. https://doi.org/10.1016/j.chom.2019.02.010.
Karakas M, Turaç-Bíçer A, Ilkit M, Durdu M, et al. Epidemiology of pityriasis versicolor in Adana. Turkey. J Dermatol. 2009;36:377–82. https://doi.org/10.1111/j.1346-8138.2009.00663.x.
Romero-Sandoval K, Alves-Costa A, Teixeira-Sousa MG, Furucho CR, et al. Recurrent and disseminated pityriasis versicolor: a novel clinical form consequent to Malassezia-host interaction? Med Hypotheses. 2017;109:139–44. https://doi.org/10.1016/j.mehy.2017.10.013.
Romano C, Mancianti F, Nardoni S, Ariti G, et al. Identification of Malassezia species isolated from patients with extensive forms of pityriasis versicolor in Siena. Italy. Rev Iberoam Micol. 2013;30:231–4. https://doi.org/10.1016/j.riam.2013.02.001.
Brandi N, Starace M, Alessandrini A, Piraccini BM. Tinea Versicolor of the neck as side effect of topical steroids for alopecia areata. J Dermatolog Treat. 2019;22:1–3. https://doi.org/10.1080/09546634.2019.1573308.
Crespo-Erchiga V, Gómez-Moyano E, Crespo M. La pitiriasis versicolor y las levaduras del género Malassezia. Actas Dermosifiliogr. 2008;99:764–71. https://doi.org/10.1016/S0001-7310(08)74956-1.
Cafarchia C, Gasser RB, Figueredo LA, Stefania M, et al. Advances in the identification of Malassezia. Mol Cell Probes. 2011;25(1):1–7. https://doi.org/10.1016/j.mcp.2010.12.003.
Honnavar P, Prasad GS, Ghosh A, Dogra S, et al. Malassezia arunalokei sp. nov., a novel yeast species isolated from seborrheic dermatitis patients and healthy individuals from India. J Clin Microbiol. 2016;54(7):1826–34. https://doi.org/10.1128/JCM.00683-16.
Hirai A, Kano R, Makimura K, Duarte ER. Malassezia nana sp. nov., a novel lipid-dependent yeast species isolated from animals. Int J Syst Evol Microbiol. 2004;54:623–7. https://doi.org/10.1099/ijs.0.02776-0.
Sugita T, Takashima M, Kodama M, Tsuboi R, et al. Description of a new yeast species, Malassezia japonica, and its detection in patients with atopic dermatitis and healthy subjects. J Clin Microbiol. 2003;41:4695–9. https://doi.org/10.1128/JCM.41.10.4695.
Sugita T, Takashima M, Shinoda T, Suto H, et al. New yeast species, Malassezia dermatis, isolated from patients with atopic dermatitis. J Clin Microbiol. 2002;40:1363–7. https://doi.org/10.1128/JCM.40.4.1363.
Petrokilidou C, Pavlou E, Gaitanis G, Bassukas I, et al. The lipid profile of three Malassezia species assessed by Raman spectroscopy and discriminant analysis. Mol Cell Prob. 2019;46:101416. https://doi.org/10.1016/j.mcp.2019.06.006.
Renati S, Cukras A, Bigby M. Pityriasis versicolor. BMJ. 2015;350:h1394. https://doi.org/10.1136/bmj.h1394.
Balestri R, Rech G, Piraccini BM, Antonucci A, et al. Pityriasis versicolor during anti TNF-a monoclonal antibody therapy: therapeutic considerations. Mycoses. 2012;55:444–6. https://doi.org/10.1111/j.1439-0507.2012.02170.x.
He S, Du W, Yang S, Zhou S, et al. The genetic epidemiology of tinea versicolor in China. Mycoses. 2017;51:55–62. https://doi.org/10.1111/j.1439-0507.2007.01437.x.
Tülin Gülec A, Demirbilek M, Seckin D, Can F, et al. Superficial fungal infections in 102 renal transplant recipients: a case-control study. J Am Acad Dermatol. 2003;49:187–92. https://doi.org/10.1067/S0190-9622(03)00861-2.
Angiolella L, Leone C, Rojas F, Mussin J, et al. Biofilm, adherence, and hydrophobicity as virulence factors in Malassezia furfur. Med Mycol. 2018;56:110–6. https://doi.org/10.1093/mmy/myx014.
• Grice EA, TLJ D. Host – microbe interactions: Malassezia and human skin. Curr. Opin. Microbiol. 2017;40:81–7. https://doi.org/10.1016/j.mib.2017.10.024An update of the immune response mechanisms in the presence of Malassezia.
Sparber F, Leibundgut-landmann S. Host responses to Malassezia spp. in the mammalian skin. Front Immunol. 2017;22. https://doi.org/10.3389/fimmu.2017.01614.
Lee WJ, Kim JY, Song CH, Jung HD, et al. Disruption of barrier function in dermatophytosis and pityriasis versicolor. J Dermatol. 2011;38:1049–53. https://doi.org/10.1111/j.1346-8138.2011.01320.x.
Tellechea Ó, Cravo M, Brinca A, Robalo-Cordeiro M. Pityriasis versicolor atrophicans. Eur J Dermatol. 2012;22:287–8. https://doi.org/10.1684/ejd.2012.1659.
Allegue F, Fachal C, Gonzáles-Vilas D, Zulaica A. Atrophying pityriasis versicolor. Actas Dermosifiliogr. 2018;109:455–7. https://doi.org/10.1016/j.ad.2017.08.013.
Marinello E, Piaserico S, Alaibac M. Atrophic pityriasis versicolor occurring in a patient with Sjögren’s syndrome. BMJ Case Rep. 2017. https://doi.org/10.1136/bcr-2016-218108.
Levy JMS, Magro C. Atrophying pityriasis versicolor as an idiosyncratic T cell-mediated response to Malassezia: a case series. J Am Acad Dermatol. 2017;76:730–5. https://doi.org/10.1016/j.jaad.2016.08.062.
• Crowson AN, Magro CM. Atrophying tinea versicolor: a clinical and histological study of 12 patients. Int J Dermatol. 2003;42(12):928–32. https://doi.org/10.1111/j.1365-4632.2003.02110.xSeries with the highest number of atrophic PV cases reported so far.
Galadari I, Komy ME, Mousa A, Hashimoto K, et al. Tinea versicolor: histologic and ultraestructural investigation of pigmentary changes. Int J Dermatol. 1992;31(4):253–6. https://doi.org/10.1111/j.1365-4362.1992.tb03565.x.
Thoma W, Krämer H, Maysert P. Pityriasis versicolor alba. J Eur Acad Dermatol Venerol. 2005;19:147–52. https://doi.org/10.1111/j.1468-3083.2004.01085.x.
Hattori M, Ogawa H, Takamori K, Gritiyaranson P, et al. De- (hypo) pigmentation mechanisms of the affected area of pityriasis versicolor. J. Dermatol. 1984;2:63–6.
Aghaei-Gharehbolagh S, Kordbacheh P, Jamal-Hashemi S, Daie Ghazvini R, et al. MGL_3741 gene contributes to pathogenicity of Malassezia globosa in pityriasis versicolor. Mycoses. 2018;61:938–44. https://doi.org/10.1111/myc.12840.
Khaddar RK, Cherif F, Hadid RB, Mokni M, et al. Penile shaft involvement in pityriasis versicolor. Acta Dermatoven APA. 2008;17:86–9.
Martínez E, Porras C, Arenas R. Pitiriasis versicolor: estudio de 194 casos con insistencia en la discromía. Dermatol Rev Mex. 2012;56:388–91.
Bonifaz A. Capítulo 8: pitiriasis versicolor. En:. In: Bonifaz A, editor. Micología médica básica. 5ª ed. México: Mc Graw Hill Education; 2015. p. 159–79.
Ramírez-Godínez JB, Carreño-Gayosso EA, Soto-Ortiz JA, Tarango-Martínez VM, et al. Pitiriasis versicolor: una actualización. Med Cutan Iber Lat Am. 2018;46:166–75.
•• Mendez A, Bonifaz A. Formas clínicas excepcionales de pitiriasis versicolor. Dermatol Rev Mex. 2019;63:347–51 A review of the atypical forms of presentation of the PV.
Goldstein BG, Goldstein AO. Tinea versicolor (Pityriasis versicolor). In: Dellavalle RP, Levy ML, Rosen T, editors. UpToDate; 2018. Retrieved aug 1, 2019, from https://www-uptodate-com/contents/tinea-versicolor-pityriasis-versicolor?search=pitiriasis%20versicolor&source=search_result&selectedTitle=1~51&usage_type=default&display_rank=1.
De Graciansky P, Mery F. Atrophie sur pityrisais versicolor aprés corticotherápie local prolongé. Bull Soc Fr Dermatol Syphiligr. 1971;78:295.
Hinojosa-Arias E, Sotelo-García L, Bonifaz A. Pitiriasis versicolor variedad atrófica: a propósito de un caso. Derma Cosmética y Quirúrgica. 2014;12:295–6.
Zawar V, Chuh A. Pityriasis versicolor imbricata – overlapping parallel scales in a novel variant of pityriasis versicolor. J Eur Acad Dermatol Venerol. 2008;22:1143–5. https://doi.org/10.1111/j.1468-3083.2007.02560.x.
Arenas R. Capítulo 96: Pitiriasis versicolor. En:. In: Arenas R, editor. Dermatología. Atlas, diagnóstico y tratamiento. 5th ed. México: Mc Graw Hill; 2013. p. 472–7.
• Mathur M, Acharya P, Karki A, Nisha K, et al. Dermoscopic pattern of pityriasis versicolor. Clin Cosmet Investig Dermatol. 2019;12:303–9. 10.2147@CCID.S195166 A description of dermatoscopic patterns in PV lesions.
Gupta AK, Foley KA. Antifungal treatment for pityriasis versicolor. J Fungi. 2015;1:13–29. https://doi.org/10.3390/jof1010013.
Gupta AK, Lyons DC. Pityriasis versicolor: an update on pharmacological treatment options. Expert Opin Pharmacother. 2014;15:1707–13. https://doi.org/10.1517/14656566.2014.931373.
• Gupta AK, Kogan N, Batra R. Pityriasis versicolor: a review of pharmacological treatment. Expert Opin Pharmacother. 2005;6:165–78. https://doi.org/10.1517/14656566.6.2.165A review of the topical and systemic treatments available for PV.
Hull CA, Johnson SM. A double blind comparative study of sodium sulfacetamide lotion 10% versus selenium sulfide lotion 2.5% in the treatment of pitiriasis (tinea) versicolor. Cutis. 2004;73:425–9.
Prestia AE. Topical benzoyl peroxide for the treatment of tinea versicolor. J Am Acad Dermatol. 1983;9:277–8. https://doi.org/10.1016/s0190-9622(83)80152-2.
Clayton R, Du Vivier A, Savage M. Double-blind trial of 1% clotrimazole cream and Whitfield ointment in the treatment of pityriasis versicolor. Arch Dermatol. 1977;113:849–50. https://doi.org/10.1001/archderm.1977.01640060145029.
Shi TW, Zhang JA, Tang YB, Yu XH, et al. A randomized controlled trial of combination treatment with ketoconazole 2% cream and adapalene 0.1% gel in pityriasis versicolor. 2015;26:143–6. https://doi.org/10.3109/09546634.2014.921661.
Sepaskhah M, Sadat MS, Pakshir K, Bagheri Z. Comparative efficacy of topical application of tacrolimus and clotrimazole in the treatment of pityriasis versicolor: a single blind, randomised clinical trial. Mycoses. 2017;60:338–42. https://doi.org/10.1111/myc.12598.
Amichai B. Treatment of pityriasis versicolor with a shampoo containing 1% bifonazole (Agispor shampoo) in children. Clin Exp Dermatol. 2000;25:660. https://doi.org/10.1046/j.1365-2230.2000.00730-6.x.
Katsambas A, Rigopoulos D, Antoniou C, Zachari A, et al. Econazole 1 % shampoo versus selenium in the treatment of tinea versicolor: a single-blind randomized clinical study. Int J Dermatol. 1996;35:667–8. https://doi.org/10.1111/j.1365-4362.1996.tb03700.x.
Sarkar S, Sengupta D, Basak S, Damji SA, et al. Comparative assessment of the efficacy of topical ketoconazole and topical luliconazole in cases of pityriasis versicolor at a tertiary care hospital in eastern India: a prospective, open, randomized controlled trial. Indian Dermatol Online J. 2016;7:335–6. https://doi.org/10.4103/2229-5178.185471.
Haroon TS, Tareen MI. An open study of tioconazole 1% dermal cream in patients with pityriasis versicolor. J Pak Med Assoc. 1984;34:361–2.
Cam VT, Van TN, Hau KT, Huu DL, et al. Efficacy of azole antifungal in treatment of pityriasis versicolor. Open Access Maced J Med Sci. 2019;7:272–4. https://doi.org/10.3889/oamjms.2019.092.
Faergemann J, Todd G, Pather S, Vawda ZF, et al. A double-blind, randomized, placebo-controlled, dose-finding study of oral pramiconazole in the treatment of pityriasis versicolor. J Am Acad Dermatol. 2009;61:971–6. https://doi.org/10.1016/j.jaad.2008.08.033.
Hald M, Arendrup MC, Svejgaard EL, Lindskov R, et al. Evidence-based Danish guidelines for the treatment of Malassezia - related skin diseases. Acta Derm Venereol. 2015;95(2015):12–9. https://doi.org/10.2340/00015555-1825.
De Souza Framil MV, Szeszs MW, Melhem MC, Zaitz C. New aspects in the clinical course of pityriasis versicolor. An Bras Dermatol. 2011;86:1135–40. https://doi.org/10.1590/s0365-05962011000600011.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Karen Adilene Camargo-Sánchez, Mirna Toledo-Bahena, Carlos Mena-Cedillos, Erika Ramirez-Cortes, Sonia Toussaint-Caire, Adriana Valencia-Herrera, Marcela Salazar-García, and Alexandro Bonifaz declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Fungal Infections of Skin and Subcutaneous Tissue
Rights and permissions
About this article
Cite this article
Camargo-Sánchez, K.A., Toledo-Bahena, M., Mena-Cedillos, C. et al. Pityriasis Versicolor in Children and Adolescents: an Update. Curr Fungal Infect Rep 13, 157–168 (2019). https://doi.org/10.1007/s12281-019-00360-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-019-00360-8