Advertisement
Advertisement
December 2022 Supplement
Sponsored by Surmodics™
Have We Found the Holy Grail for Thromboembolectomy?
A conversation with Dr. Gary Ansel, inventor of the Pounce™ Thrombectomy System.
Throughout his 36 years as a physician, Gary Ansel, MD, has focused on overcoming challenges in endovascular medicine—not only as a renowned interventional cardiologist and clinical investigator but as a medical device inventor and entrepreneur. Among his medical device brainchildren are the Flexor® Ansel Guiding Sheath, one of the world’s most-utilized interventional sheaths, and the Pounce™ Thrombectomy System, recently introduced by Surmodics, Inc. for removal of thrombi and emboli from the peripheral arterial vasculature. We spoke with Dr. Ansel about why he set out to design and develop what became the Pounce™ Thrombectomy System and why he believes it will have a profound impact on patient outcomes and clinical practice.
You’ve said that new medical devices must provide a really good answer to a big need. What big need does the Pounce™ Thrombectomy System address?
We need to make it easier for more physicians, across specialty lines, to remove arterial thrombi and emboli right on the angiographic table, without transferring patients to tertiary care centers. I saw this need very clearly when I was the Health System Medical Chief for the vascular program at OhioHealth (Columbus, Ohio). When we can’t remove clot during the initial percutaneous procedure, the patient typically undergoes thrombolysis, permanent implantation of a stent, or referral for open surgery for thrombectomy or bypass. All these events add time and cost and lead to increased risk of complications and death.
In practical terms, we’ve long needed a stand-alone thrombectomy device that is easy to use and can provide safe, single-session removal of the full breadth of arterial thrombi and emboli interventionalists encounter in patients in real-world settings. By that, I mean mixed, organized thrombus, not just the soft stuff. That’s what the Pounce™ Thrombectomy System does.
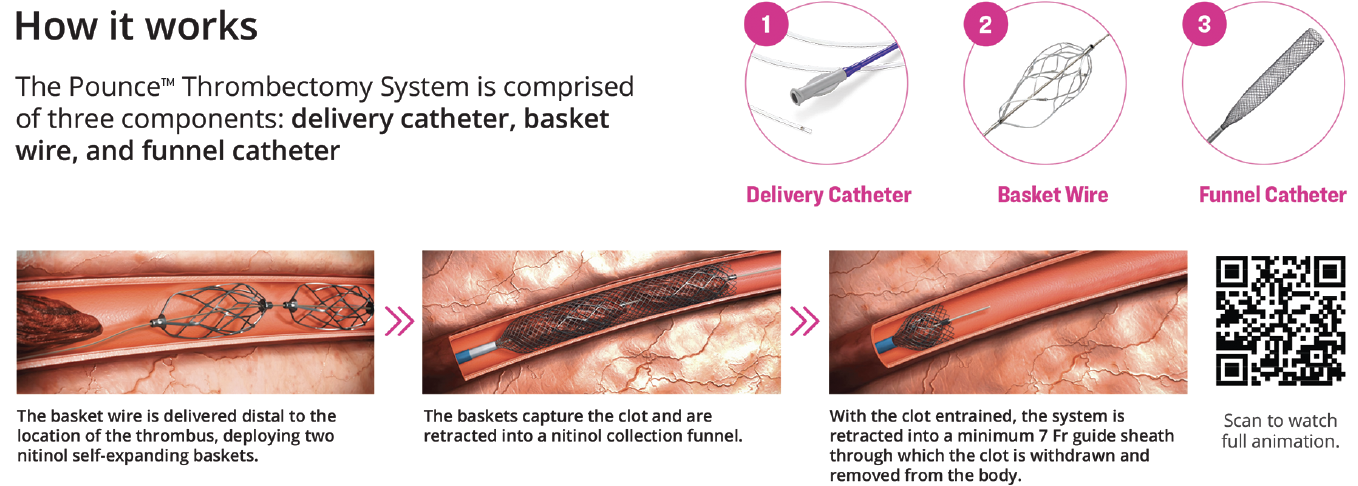
How does the Pounce™ Thrombectomy System work?
It’s simple. Basically, I wanted a percutaneous device that could do what a Fogarty® catheter does but without the need for a surgical incision. With the Pounce™ System, you percutaneously place the basket wire distal to the clot, place the collection funnel proximal to the clot, pull back on the basket wire, collect the thrombus in the funnel, and pull out the clot (Figure 1). The Pounce™ Thrombectomy System is designed to macerate and dehydrate the clot, making it easy to remove large quantities of material through a small 7 Fr sheath.
Where do you think other thrombectomy devices fall short?
In my experience, aspiration-based thrombectomy devices only work well on soft thrombus. Tougher clots are a real problem for them. That’s why aspiration-based devices are rarely a stand-alone solution. The more aggressive devices, which also handle atheroma, are associated with increased risk of complications such as perforation.1 Even today, most recommendations call for open surgery for an arterial embolus,2 despite the minimal invasiveness and time savings of endovascular techniques. I believe this reflects the historical inadequacies of the percutaneous devices we’ve had available.
What clinical data have been published or presented on the Pounce™ Thrombectomy System to date?
Data on the first 20 consecutive patients were presented at the Charing Cross (CX Symposium International) 2022 meeting.3 The patients included acute onset to chronic symptoms up to 8 months. The length of occlusion ranged from 5 to 300 mm. There was 100% on-table target lesion success, and the average procedure time was less than 90 minutes. No adjunctive thrombectomy treatments were required for thrombus treatment in the target vessels. Really very impressive results, especially when you consider that these initial, consecutive cases included any physician learning curve for the device.
What else have you learned from observing the Pounce™ Thrombectomy System in clinical use?
What’s been really surprising is how effective we’ve seen Pounce™ work on thrombotic chronic total occlusions, the longest so far being 8 months. As a strategy, we’ve found that if a hydrophilic wire easily traverses an occlusion, which signifies a soft thrombotic core, physicians have been able to remove most of the angiographic occlusion made up of chronic thrombus, thereby shortening the treatment area due to the offending atherosclerotic lesion. The underlying atherosclerosis can then be simply treated with traditional means such as drug-coated balloons or stents with minimal concern for embolization. Honestly, the Pounce™ Thrombectomy System has exceeded my design expectations.
What were your original design specifications for the Pounce™ Thrombectomy System?
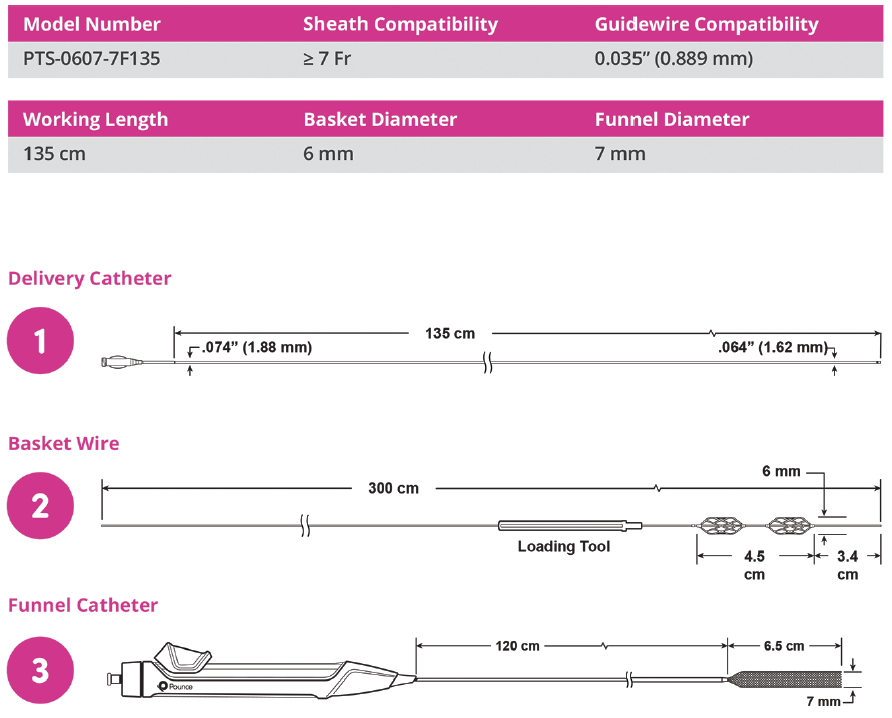
There were several areas that needed to be addressed. First, it had to be safe and simple to use by the breadth of interventional physicians and consistently provide on-table results without the need for additional devices, thrombolysis, or open surgical cutdowns. As an interventionalist myself, I felt that we should have a simple device that typically requires less than an 8 Fr sheath and does not aspirate or remove blood (Figure 2). I was also tired of the complex process of getting a capital purchase approved. I wanted something you could just grab and use without a console to be rolled into the room.
These were lofty goals, and we’ve been through a lot of blood, sweat, and tears to get to where we are now. The path from concept to market for this device began around 2009, and it wasn’t for the faint of heart.
Why did you set a goal of less than 8 Fr size?
My experience is that there is not much difference between a 6 Fr and a 7 Fr sheath for crossing an aortic bifurcation or in terms of closure device outcomes. In my experience, once you go to 8 Fr, you reduce the success rate and increase the complication rate for your arterial procedures. As you increase French sizes, you also decrease the number of patients that can undergo a given procedure, because some patients can’t tolerate a bigger sheath due to vessel diameter and aortic bifurcation angulation. That’s why I thought 7 Fr was an important goal from the outset.
Explain why you were opposed to using aspiration.
Blood loss has been demonstrated to be associated with poorer patient outcomes. Often, the patients we treat also have anemia. When removing significant amounts of blood during an aspiration thrombectomy, an operator must balance time of aspiration, and thus blood loss, with needed effect. Clearly, transfusions are undesirable because of their inherent risks, and they’re a quality marker for a hospital. Significant anemia may take a month or more to resolve and patients feel terrible during that time—not desirable for patient experience surveys, which have become more and more important.
What was the biggest challenge you faced in meeting the goals you set for the Pounce™ Thrombectomy System?
Being true to the design criteria I developed, especially in striking the right balance between device size and thrombotic mass removal. When the team developed a funnel that could macerate and dehydrate the thrombus, the amount of clot needing removal decreased significantly. The funnel is the secret sauce.
Why two baskets on the basket wire and not one?
I wish I could tell you that two baskets was the first thought. Again, we were trying to mimic the approach of a Fogarty® catheter. Through trial and error, we found that efficiency dramatically improved with the second basket.
The Pounce™ Thrombectomy System is a fixed-wire system. What has been the early experience with crossing and re-crossing thrombotic occlusions?
I can understand why some physicians may be concerned about wire loss, but our experience has shown that after the first pass, subsequent wire passage becomes easier because you’ve developed a channel for the subsequent guidewire passage if needed. This is what Dr. Bruce Gray’s team found in their first 50 cases using the Pounce™ Thrombectomy System (see Dr. Gray’s article in this supplement).
What has been the early experience with embolization with the Pounce™ Thrombectomy System?
The dual baskets and double-wire funnel work together and were designed to have a low risk of embolization. Distal embolization has not been an issue to date.
COVID-19 has placed a lot of stress on health care systems. How does the Pounce™ Thrombectomy System fit into this picture?
Even before COVID, health care systems were facing a workforce problem, with projected shortages of physicians and staff. Then COVID came along, and we were faced with an acute shortage of technologists and nurses. This has led to disruption of traditional support teams and frequent use of contract personnel, which can really impact complex procedures such as acute limb ischemia. All these conditions make it incumbent for new medical devices to be simple and straightforward to use, with short learning curves. We’ve also seen that hospitals have become reluctant to invest in devices that require capital purchase and ongoing service agreements. The Pounce™ Thrombectomy System requires no capital purchase and was designed to be inherently simple to use and easily understood by the physician and the staff.
1. Zeller T, Müller C, Frank U, Bürgelin K, Horn B, Roskamm H. The Straub-Rotarex thrombectomy system: initial experiences. Rofo. 2001;173:626-631. doi: 10.1055/s-2001-15843
2. de Athayde Soares R, Matielo MF, Neto FCB, et al. Analysis of the results of endovascular and open surgical treatment of acute limb ischemia. J Vasc Surg. 2019;69:843-849. doi: 10.1016/j.jvs.2018.07.056
3. Ansel GM. Presented at the 44th Charing Cross Symposium; April 22, 2022; London, United Kingdom.

Caution: Federal (US) law restricts the Pounce™ Thrombectomy System to sale by or on the order of a physician. Please refer to the product Instructions for Use for indications, contraindications, warnings, and precautions.
SURMODICS, POUNCE, and SURMODICS and POUNCE logos are trademarks of Surmodics, Inc. and/or its affiliates. Third-party trademarks belong to their respective owners.
Advertisement
Advertisement